Note: The Pregistry website includes expert reports on more than 2000 medications, 300 diseases, and 150 common exposures during pregnancy and lactation. For the topic Vitamin A Deficiency, go here. These expert reports are free of charge and can be saved and shared.
_________________________________
Here on The Pulse, we have discussed a lot about vitamin D and about vitamins overall during pregnancy, but not so much about vitamin A, so let’s make vitamin A our topic for today.
In 2017, the World Health Organization (WHO) reported that approximately 19 million pregnant women in developing countries suffer from vitamin A deficiency (VAD), meaning a deficiency of vitamin A , which scientists also call all-trans-retinol. This is a fat-soluble vitamin that is vital, both to pregnant women and their developing babies.
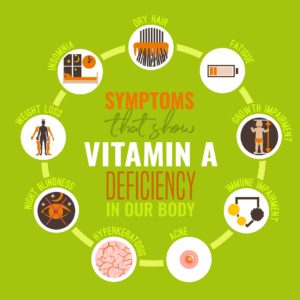
Vitamin A plays a major role in bone the skeletal system (bones) and in various organs, but is particularly crucial for the development of the eye. Diagnosis of VAD thus requires an ophthalmologist, or an optometrist. Eye examination reveals very specific abnormalities, namely xerosis (dry eyes), corneal ulceration and melting (kerotomalacia), retinopathy (abnormalities of the retina, the part of the eye where images are generated and converted into nervous signals), and night blindness (nyctalopia). Worldwide, VAD is the number one preventable cause of blindness and because of the needs of the growing fetus, your requirements for vitamin A are more during pregnancy than when you are not pregnant. Therefore, VAD can be a problem if you don’t receive adequate amounts of vitamin A, or a precursor to vitamin A such as beta carotene in your diet. Mild VAD may be subclinical (not causing symptoms) or it can give you night blindness (nyctalopia). If the deficiency progresses and is not treated, this can lead to permanent blindness. Non-ocular effects of VAD include dry skin, delayed or inadequate wound healing, exacerbation of acne, anemia, and problems with the immune system, leading to severe throat infections and very difficult-to-treat types of pneumonia that can be fatal. In addition to problems for the mother, VAD during pregnancy can lead to a variety of adverse outcomes for the baby, such as low birth weight, preterm birth, small for gestational age, and fetal loss, plus it elevates the risk of neonatal or infant death.
The treatment for VAD is vitamin A. Mild to moderate VAD with symptoms can be treated with up to 10,000 IU (3,000 mcg) per day. In non-pregnant adults, severe VAD can be treated with therapeutic vitamin A doses up to 200,000 IU (60,000 mcg) daily, but such doses are thought to cause birth defects. Consequently, WHO guidelines recommend that pregnant women are given no more than 10,000 IU, or a weekly dose of 25,000 IU. If you suffer from VAD while pregnant, you should not exceed the limit of vitamin A dosage recommended by WHO, but you should not discontinue the therapy until your doctor tells you to do so. WHO recommendations all a vitamin A daily dose of 200,000 IU for lactating mothers who have severe VAD. Be aware that this is much higher than the limit that is recommended during pregnancy.
If your VAD is subclinical, meaning that you do not suffer very noticeable symptoms, you may be able to avoid vitamin A in pills and increase your vitamin A levels by consuming foods that are rich in vitamin A, such as beef, liver, chicken, eggs, and fortified milk, and foods that are rich in beta carotene, such as cantaloupe, tomatoes, and mangoes. Consumption of food rich in vitamin A or beta carotene is also vital for preventing VAD and its complications. One very promising development against VAD on a large scale is Golden Rice, a rice that has been genetically engineered to make beta carotene. This is a non-profit program funded by the Bill and Melinda Gates Foundation and potentially, it can prevent blindness and death in millions of people, including many children, in places where rice dominates the diet. However, due to misinformation spread by organizations opposed to biotechnology, including various food companies and non-governmental organizations that have been pushing an increasing number of so-called “non-GMO” food products into consumer markets.