Gastroesophageal disease, also known as GERD, affects about 60 percent of the population at least once a year, but up to 80% of all pregnant women report GERD symptoms such as heartburn.
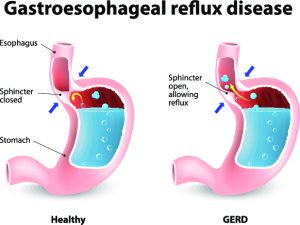
GERD happens when stomach acid flows back into your esophagus, the muscular tube that connects your throat and stomach. The reason it happens more often during pregnancy is that changes in hormone levels slow down the muscles responsible for digestion, including those muscles that move food through your esophagus. Later on in pregnancy, the growing baby can press against abdominal organs, forcing stomach acid back up into the esophagus.
While most women experience some indigestion during pregnancy, a few factors can increase the likelihood of developing more frequent and severe symptoms.
The number one risk factor for having frequent and severe symptoms during pregnancy is having GERD symptoms before you become pregnant. Other risk factors include maternal age and the amount of weight gained during pregnancy. The more weight gained, the higher the risk of developing GERD.
Treating GERD—whether or not you are pregnant—usually starts by making some lifestyle modifications. Here are a few modifications that your doctor may prescribe:
- Eat smaller meals. Being too full can prompt symptoms.
- Eat slowly and chew your food carefully.
- Don’t eat just before bedtime. Aim to have your last meal at least three hours before you normally go to bed.
- Don’t lie down directly after a meal, even a light one.
- Don’t smoke. One of the many reasons not to smoke is that smoking weakens esophageal muscles.
- Avoid trigger foods such as caffeine, fried, fatty or spicy foods. If you’re not sure which foods trigger symptoms, keep a food diary.
- Use a nursing pillow or foam wedge to raise your head six to eight inches while sleeping.
- Sleep on your left side.
- Bend at the knees rather than bending at the waist. Don’t bend at all right after eating.
- Chew gum.
Relief can sometimes be obtained by using natural remedies. Here are a few remedies that women have found helpful. However, the fact that the remedies are natural does not necessarily mean they are recommended during your pregnancy. Always discuss the use of any remedies with your doctor.
- Ginger tea
- Apple cider vinegar. Mix two to three teaspoons of apple cider vinegar into in an eight-ounce glass of water.
- Baking soda. Mix one tablespoon of baking soda into a half cup of water.
Should symptoms not respond to lifestyle modifications, over-the-counter antacids may help. The use of over-the-counter medications should also be discussed with your doctor. The fact that they are sold over the counter does not mean they won’t have implications during your pregnancy.
For example, antacids that contain calcium can reduce the absorption of iron and should be taken at a different time of the day from your iron supplement. Magnesium-containing antacids can slow contractions, although the effect varies from woman to woman.
If GERD symptoms persist and are severe, discuss further treatment options with your doctor. Except for omeprazole, commonly marketed as Prilosec, the US Food and Drug Administration (FDA) has classified all proton pump inhibitors (PPI) used to treat GERD as category B drugs, which means they are safe to use during pregnancy. Omeprazole is a class C drug, which means that animal studies have demonstrated risk but human studies have not been conclusive. Several studies of pregnant women taking omeprazole have found no risk.
Some healthcare providers recommend temporarily discontinuing PPIs while you are pregnant and some studies suggest you should stop treatment if you are planning to become pregnant.
Heartburn and other GERD symptoms rarely result in any pregnancy complications. However, you should call your doctor if you:
- Feel as if food is stuck in your throat
- Continue to have symptoms that do not respond to lifestyle modifications
- Have a fever or vomit
- Experience chest pain
GERD symptoms usually improve after the baby is born. If you do experience symptoms in the weeks after giving birth, your doctor may order testing to screen out an underlying problem.